Recently, it was International Keratoconus Awareness Day on November 10th. I thought I’d write up a short post about keratoconus (KC), as it’s a condition that’s sort of near and dear to my heart. Most folks have never heard of KC because it’s just not something that gets brought up until you have it. You probably know someone with it or even have a family member who has it and they’ve just never mentioned it to you before.
KC is a condition which affects the cornea, the front portion of the eye. Normally this area is meant to be perfectly rounded. If it’s flatter in area and steeper in another, this leads to astigmatism (which you can read about here).
However, what happens in KC is the cornea begins to become thinner over time and start to droop. No longer is it perfectly round and providing a normal surface for light to bend to the back of the eye, but instead causes light to randomly scatter leading to blurred vision.
In many cases, early KC will just appear like an increase in astigmatism without anything else to warn us. It tends to be more prominent in patients who rub their eyes aggressively, patients with atopic conditions (eczema, psoriasis, asthma, etc), or in patients with a family history of KC.
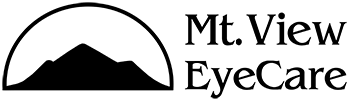
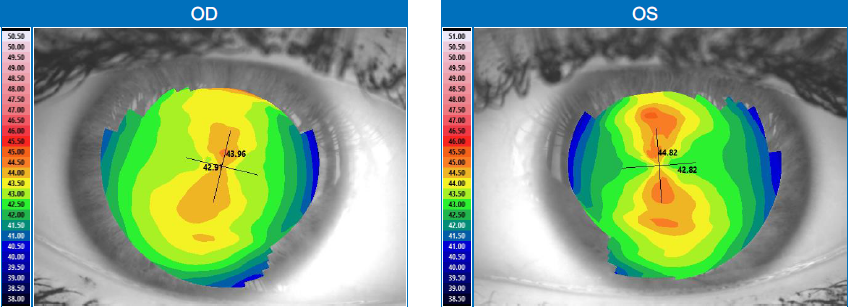
Below are topographical maps of a normal cornea and a cornea with KC. The first maps you can see that there is a bit of a figure eight or bowtie pattern to them. This is what normal astigmatism looks like. The warmer the colors are, the steeper that area is.
Normal Cornea
Cornea with KC
The second topography, you see just a large island of red lower down on the map. This is because the cornea has become thin and began to droop down with more advanced KC. Because the cornea has become irregular, this is why glasses typically do not work well for patients with KC. Many get little to no improvement.
In younger patients, the condition can progress rapidly and lead to major vision loss within months if not treated early. Sadly, some patients don’t realize something is wrong until it’s more advanced. I have had patients who told me they were seeing perfectly 6 months ago and suddenly now they can’t see, only to be diagnosed with KC.
Most of the time when KC has progressed to causing vision problems, patients are not able to see 20/20 with glasses alone. Many patients benefit from special types of contact lenses, like scleral, hybrid or rigid gas permeable (RGP lenses) to restore them with somewhat normal levels of vision.
We specialize in fitting these kinds of lenses at Mt. View EyeCare. This is probably the biggest reason I feel this condition is near and dear to me. We receive many referrals for patients with the condition to test out contact lenses and see if they can have quality of life improvement because many patients just give up on being able to see. Some of my patients come in feeling absolutely hopeless that they’ll never see better than 20/100 leave crying because after we fit them in contacts they can see 20/30 (In some cases better) and feel like they have their life back.
Prior to 2016, there was no FDA approved method of treatment for KC other than awaiting needing a transplant or placing rigid plastic rings in the cornea. A transplant is typically seen as a last resort option, while the plastic rings were seen as a stop gap that might be beneficial, but might not.
Thankfully, the FDA finally approved corneal cross linking (CXL) after many years of study in the US, as well as data from Canada and Europe showing it was a beneficial procedure. The goal with KC is that now patients can receive CXL early on in the condition and slow down the progression or halt it altogether. While CXL isn’t a cure, it is hope that many patients who would have progressed to needing a transplant can remain stable without the need of transplant in the coming years.
Below is a link to a PDF from “Living with Keratoconus.” The website is owned by the manufacturer of the laser used for CXL, but I still found the PDF to contain some good images and content regarding keratoconus. Some of the pictures show exaggerated portrayals of what the cornea looks like, but it gives a better idea of what it can look like!
If you or someone you know has a history of keratoconus, please feel free to give us a call anytime. We are happy to test out some contact lenses for you to see if we can improve your comfort and vision. If you are interested in cross linking, we work with some of the best corneal specialists in the entire country in Portland to help patients get the procedure when it’s necessary.
https://www.livingwithkeratoconus.com/wp-content/uploads/2019/07/LWKC_Keratoconus-Infographic.pdf
Nick Jankowski, OD
Mt. View EyeCare Center